
Progress
and
Pitfalls
in
Underrepresented
Minority
Recruitment:
Perspectives
from
the
Medical
Schools
Jaya
R.
Agrawal,
MD,
MPH;
Sorina
Vlaicu,
MD,
PhD;
and
Olveen
Carrasquillo,
MD,
MPH
Boston,
Massachusetts;
Arlington,
Virginia;
and
New
York,
New
York
Financial
support:
Funding
from
the
Office
of
Minonty
Health
of
the
Department
of
Health
and
Human
Services
(OMH)
and
the
American
Medical
Student
Association
(AMSA).
Dr.
Carrasquillo's
effort
on
this
project
was
supported
by
a
Cen-
ter
of
Excellence
Grant
from
the
National
Center
for
Minority
Health
and
Health
Disparities
(NCMHD,
MD00206
P60).
Purpose:
To
assess
current
initiatives
at
U.S.
medical
schools
to
recruit
underrepresented
minorties
(URM)
and
to
identify
perceived
barriers
to
enrollment
of
URM
students.
Methods:
We
developed
a
survey
that
was
mailed
to
the
dean
of
Student
Affairs
of
all
U.S.
allopathic
and
osteopathic
medical
schools
in
2002.
Respondents
were
asked
to
list
their
schools'
URM
recruitment
programs
and
rate
the
effective-
ness
of
these
programs.
They
were
also
asked
to
indicate
barriers
to
URM
recruitment
from
a
list
of
37
potential
barriers
and
rate
their
overall
success
with
URM
recruitment.
Results:
The
study
had
a
59%
response
rate.
All
schools
report-
ed
a
wide
varety
of
initiatives
for
URM
recruitment
with
.50%
of
all
schools
using
each
of
the
11
strategies.
The
three
most
commonly
listed
barriers
to
URM
recruitment
were
MCAT
scores
of
applicants
(90%),
lack
of
minority
faculty
(71%)
and
lack
of
minority
role
models
(71%).
Most
schools
rated
their
recruitment
efforts
highly;
on
a
scale
of
1
to
10
(10
being
very
successful),
the
average
score
was
an
8.
Conclusion:
While
schools
continue
to
invest
tremendous
efforts
in
recruiting
minorty
applicants,
admissions
crtera,
lack
of
URM
faculty
and
the
need
for
external
evaluation
remain
important
bariers
to
achieving
a
diverse
physician
workforce.
Key
words:
underrepresented
minorities
*
medical
school
admissions
©
2005.
From
the
Deportment
of
Medicine,
Brigham
and
Women's
Hospital,
Boston,
MA
(Agrawal);
the
School
of
Public
Policy,
George
Mason
University,
Arlington,
VA
(Vlaicu,
presently
at
The
University
of
Western
Ontario,
London,
Ontario,
Canada)
and
the
Center
for
the
Health
of
Urban
Minorities,
Colum-
bia
University
Medical
Center,
New
York,
NY
(Carrasquillo).
Send
correspon-
dence
and
reprint
requests
for
J
NotI
Med
Assoc.
2005;97:1226-1231
to:
Olveen
Carrasquillo,
MD,
MPH,
Division
of
General
Medicine,
Columbia
Uni-
versity
Medical
Center,
PH
9E
Room
105,
622 W.
168th
St.;
phone:
(212)
305-
9782;
fax:
(212)
305-9349;
e-mail:
BACKGROUND
Despite
nearly
a
quarter
century
of
diversity
ini-
tiatives
by
government
agencies,
medical
schools
and
other
organizations,
the
percentage
of
medical
students
who
belong
to
historically
underrepresent-
ed
racial
and
ethnic
minority
(URM)
groups
has
remained
fairly
uniform,
fluctuating
from
8.0%
to
12.5%,'
while
representation
of
these
same
minority
groups-African
Americans,
Hispanic
Americans
and
Native
Americans-in
the
U.S.
population
has
reached
26%
and
continues
to
grow.2
The
Sullivan
Commission
on
Diversity
in
the
Health
Workforce
concluded
"failure
to
reverse
these
trends
could
place
the
health
of
at
least
one-
third
of
the
nation's
citizens
at
risk."3
Furthermore,
the
Institute
of
Medicine
(IOM)
has
recommended
"institutional
and
policy
level
change"
aimed
at
increasing
the
proportion
of
URMs
among
the
health
professions
as
part
of
a
multifaceted
strategy
to
reduce
racial
and
ethnic
disparities
in
healthcare.4
Understanding
the
causes
of
difficulties
in
recruit-
ment
of
URM
students
has
been
the
focus
of
much
commentary
and
limited
empirical
analyses.
We
con-
tribute
to
this
work
through
a
national
survey
of
med-
ical
schools
that
aims
to
assess
self-reported
efforts
by
the
medical
schools
to
recruit
URM
students,
iden-
tify
barriers
which
the
schools
report
in
recruiting
URM
students
and
examine
the
opinions
of
adminis-
trators
regarding
their
success
at
URM
recruitment.
The
only
other
similar
survey
of
which
we
are
aware
is
the
2004
study
by
Dinan
et.
al.,
commissioned
by
the
Sullivan
Task
Force.3
However,
they
were
only
able
to
obtain
limited
data
from
most
schools,
and
the
focus
of
their
analysis
was
on
the
subset
of
14
medical
schools
they
identified
as
having
innovative
programs
aimed
at
increasing
diversity.
METHODS
Instrument
Development
In
developing
the
American
Medical
Student
Association
Diversity
Survey
(AMSA-DS),
we
first
1226
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
97,
NO.
9,
SEPTEMBER
2005

UNDERREPRESENTED
MINORITY
RECRUITMENT
conducted
a
review
of
the
relevant
literature
using
a
Medline
search
for
combinations
of
the
following
key
words:
"underrepresented
minorities,"
"medical
school
admissions,"
"diversity,"
"recruitment,"
"retention"
and
"representation."
Included
were
all
articles,
both
research
studies
and
commentary,
pub-
lished
between
1985
and
2000
and
having
any
dis-
cussion
of
minority
representation
in
medical
schools.
A
summary
of
the
findings
in
these
articles
with
an
annotated
bibliography
were
presented
to
AMSA's
Diversity
Coalition,
a
group
of
eight
mem-
bership-based
medical
associations
with
a
stated
commitment
to
diversity
in
their
mission
statement
(Tablel).
Representatives
of
these
organizations
drafted
the
AMSA-DS.
In
the
fall
of
2001,
the
instrument
was
pilot-tested
at
four
medical
schools.
The
deans
of
students
at
each
of
these
schools
were
asked
to
comment
on
content,
length
and
clarity
of
the
survey
and
survey
items.
Based
on
their
feed-
back,
the
instrument
was
revised
by
modifying
some
questions,
adding
certain
items
and
excluding
other
questions.
The
final
survey
contained
100
items
and
took
approximately
20
minutes
to
complete
[instru-
ment
available
from
Carrasquillo
(author)].
Survey
items
included:
1.
A
list
of
37
potential
barriers
to
URM
recruit-
ment
with
respondents
being
asked
to
check
all
that
applied
to
their
school;
2.
A
list
of
11
URM
recruitment
programs
with
respondents
being
asked
to:
a)
note
whether
the
program
was
in
place
at
their
institution
and
b)
rate
the
effectiveness
of
the
program
by
using
a
modified
four-point
Likert
scale
(not
effective,
effective,
very
effective
and
don't
know).
The
survey
also
included
one
question
asking
for
an
overall
assessment
of
the
school's
success
in
the
recruitment
of
URM
students
on
a
scale
of
1
to
10
(10
being
best).
Lastly,
we
undertook
this
project
during
a
nationwide
discussion
led
by
the
Association
of
American
Medical
Colleges
on
redefining
and
expanding
the
term
"underrepre-
sented
minority."
Therefore,
an
additional
ques-
tion
asked
medical
schools
if
they
would
like
to
target
for
recruitment
any
of
several
listed
addi-
tional
minority
and
disadvantaged
groups
[other
minorities
(e.g.
Asians,
non-URM
Hispanics),
women,
gay/lesbian/transgender
students,
dis-
abled,
economically
disadvantaged,
second-
career
professionals
and
an
open-ended
question
on
other
groups].
In
spring
2002,
we
mailed
the
AMSA-DS
and
an
accompanying
letter
signed
by
the
presidents
of
AMSA
and
the
Student
National
Medical
Associa-
tion
(SNMA)
to
the
deans
of
student
affairs
of
all
144
accredited
allopathic
and
osteopathic
medical
schools.
Deans
were
asked
to
identify
their
school
by
name
for
purposes
of
follow-up
only,
with
assur-
ance
of
confidentiality.
In
many
cases,
the
survey
was
forwarded
to
the
dean
of
admissions
or
minority
affairs
faculty
who
responded
to
the
survey.
A
post-
card
reminder
was
sent
at
the
four-week
mark
and
the
instrument
was
faxed
to
schools
at
the
eight-
week
mark
with
telephone
follow-up.
Schools
responded
to
the
instrument
via
mail
or
fax.
The
data
collection
period
was
closed
10
weeks
after
the
ini-
tial
mailing.
Surveys
were
collected
by
independent
consultants
at
the
School
of
Public
Policy
at
George
Mason
University
and
entered
into
a
database
with
identifying
information
removed.
Because
the
goal
of
the
study
was
to
assess
the
viewpoints
and
efforts
of
schools
struggling
with
enrollment
of
traditional
URM
students,
we
did
not
include
schools
who
already
enrolled
a
high
proportion
of
URM
students.
Thus,
schools
indicating
that
they
were
a
historically
black
medical
school
or
located
in
Puerto
Rico
were
excluded
from
this
analysis.
Statistical
Analysis
We
compared
differentials
in
characteristics
among
responding
and
nonresponding
medical
schools
using
Chi-squared
analyses.
We
analyzed
the
percentage
of
URM
students
at
each
school
as
a
continuous
variable,
and
correlates
of
URM
enroll-
ment
with
categorical
variables
were
examined
using
t
tests
with
Bonferoni
adjustment
for
multiple
comparisons.
We
present
descriptive
data
on
exist-
ing
initiatives
at
medical
schools
to
recruit
URM,
perceived
barriers
to
enrollment
of
URM
and
inter-
est
in
recruiting
other
minority
students
as
percent-
ages.
Self-reported
success
at
recruiting
URM
stu-
dents
was
not
normally
distributed
(as
determined
with
visual
examination
of
data
plots
and
the
Wilk-
Shapiro
test).
Thus,
we
used
Spearman
correlation
coefficients
to
examine
the
association
between
self-
reported
success
and
the
percentage
of
URM
stu-
dents
at
each
school.
All
analyses
were
performed
using
SAS
v8.
Table
1.
Organizations
that
participated
in
the
American
Medical
Student
Diversity
Coalition
1.
Student
National
Medical
Association
2.
National
Medical
Association
3.
National
Network
of
Latin
American
Medical
Students
4.
National
Hispanic
Medical
Association
5.
American
Medical
Student
Association
6.
American
Medical
Women's
Association
7.
Association
of
American
Indian
Physicians
8.
Gay
and
Lesbian
Medical
Association
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
97,
NO.
9,
SEPTEMBER
2005
1227

UNDERREPRESENTED
MINORITY
RECRUITMENT
RESULTS
The
overall
response
rate
was
59%
(86
out
of
144),
which
compares
favorably
with
the
41%
response
rate
obtained
by
Dinan
et. al.
in
their
medical
school
sur-
vey.4
Our
response
rate
did
not
differ
by
geographic
region
but
was
higher
among
osteopathic
schools
than
allopathic
schools
(68%
versus
55%,
P<0.05).
Of
the
responding
institutions,
50
identified
themselves
as
public
and
28
as
private;
eight
schools
did
not
respond
to
this
survey
question.
Among
the
60
schools
respond-
ing
to
the
question
on
the
percentage
of
entering
stu-
dents
who
were
URM,
the
mean
was
10.4%
(median
10.0,
inter-quartile
range
6-15%).
This
figure
is
similar
Table
2.
Medical
school
reported
barriers
to
underrepresented
minority
recruitment
Barrier
Percent
Listing
as
Barrier
at
Their
Institution
Legal/Policy/Regulatory
Court
decisions
33%
State/local
policies
19%
State
legislation
limiting
affirmative
action
14%
Educational
Low
MCAT
scores
90%
Low
undergraduate
GPA
60%
Poor
preparation
in
sciences
55%
Absence
of
high
school
science
interest
programs
46%
Low
educational
achievement
40%
Lower
quality
of
schools
previously
attended
34%
Lower
level
of
academic
achievement
among
parents
30%
Poor
communication
skills
19%
No
participation
in
service-oriented
extracurricular
activities
17%
Socio-cultural
Absence
of
role
models
77%
Lack
of
peer/community
support
45%
State/area
population
not
diverse
37%
Negative
parental
and
cultural
attitudes
regarding
careers
19%
Financial/Economic
Lack
of
financial
aid
48%
Parental
income
level
39%
Difficulties
in
finding
financial
resources
for
your
school's
programs
28%
No
financial
travel
assistance
to
the
required
admission
interview
27%
High
application
fees
14%
Housing
issues
12%
Recruitment/Admission
Not
enough
minority
faculty
members
71%
Other
schools
in
the
area
targeting
URM
majoring
in
sciences
39%
Absence
of
summer
enrichment
programs
at
your
school
27%
Race/ethnicity/gender
composition
of
the
admission
committee
22%
Absence
of
partnerships
with
private
and
public
organizations
20%
Lack
of
mentorship
programs
20%
Lack
of
career
development
outreach
16%
No
URM
student
recruiters
13%
Complex
application
process
10%
No
pre-admission
counseling
and
application
assistance
7%
Absence
of
an
office
of
minority
and/or
multicultural
affairs
7%
No
faculty
member
designated
to
address
issues
of
concern
from
URM
students
7%
to
the
10.9%
URM
enrollment
at
all
U.S.
medical
schools
in
2001.1
The
mean
percentage
of
URM
did
not
differ
significantly
among
private
schools
versus
pub-
lic
schools
or
at
osteopathic
versus
allopathic
schools.
Phone
contact
with
nonresponding
schools
found
that
that
lack
of
time
or
staff
resources
to
fill
out
the
survey
by
the
deadline
was
the
most
common
reason
for
lack
of
participation.
However,
two
schools
expressed
con-
cern
that
providing
data
on
this
topic
would
leave
them
legally
vulnerable.
Barriers
to
Recruiting
Minority
Students
Of
the
37
possible
barriers
to
URM
recruitment,
1228
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
97,
NO.
9,
SEPTEMBER
2005
UNDERREPRESENTED
MINORITY
RECRUITMENT
only
five
were
cited
as
significant
by
at
least
half
of
the
responding
schools
(Table
2).
Of
these,
three
barriers
were
related
to
educational
preparation,
with
low
MCAT
scores
being
mentioned
by
90%
of
schools.
The
other
commonly
listed
educational
barriers
were
low
grade
point
average
(GPA)
(60%)
and
poor
preparation
in
the
sciences
(55%).
However,
the
second
and
third
most
commonly
listed
barriers
to
URM
recruitment
were
related
to
minority
faculty
representation
in
the
medical
school.
In
fact,
the
absence
of
role
models
and
lack
of
minority
faculty
members
were
noted
as
signif-
icant
barriers
by
three-quarters
of
respondents.
Financial
barriers
were
cited
by
less
than
half
of
respondents,
and
on
the
whole,
schools
did
not
feel
that
their
recruitment
process
or
institutional
quali-
ties
posed
a
problem-with
the
exception
of
lack
of
minority
faculty
members.
Interestingly,
although
our
study
was
conducted
prior
to
the
Supreme
Court's
recent
favorable
ruling
on
affirmative
action,
even
before
this
ruling,
less
than
one-third
of
respondents
cited
legal
issues
around
affirmative
action
as
a
significant
barrier.
Recruitment
Strategies
We
found
that
most
schools
have
a
wide
variety
of
initiatives
for
URM
recruitment
(Table
3).
Indeed,
each
of
the
11
URM
recruitment
strategies
listed
in
our
survey
were
present
in
at
least
half
of
the
schools.
Of
these,
preadmission
site
visits
to
med-
ical
schools
by
minority
applicants
(91%),
pre-
admission
counseling
(88%),
career
outreach
pro-
grams
to
communities
(83%),
financial
aid
(82%)
and
URM
student
early
identification
(77%)
were
the
most
commonly
utilized.
When
asked
to
rate
the
effectiveness
of
each
of
the
recruitment
programs
employed
by
their
schools,
less
than
half
of
the
schools
gave
any
of
these
specific
strategies
the
highest
rating
of
"very
effective",
with
two
notable
exceptions:
URM
student
recruiters
(61%
of
schools
rated
this
recruitment
strategy
as
"very
Table
3.
Medical
school
reported
recruitment
strategies
for
underrepresented
minority
students
Recruitment
Strategy
Percent
of
Schools
Percent
Rating
Program
with
Program
Very
Effective
Site
visit
to
school
(pre
admission)
91%
44%
Pre-Admission
Counseling
87%
40%
Career
development
outreach
in
primary
or
secondary
schools
81%
30%
Financial
Aid
80%
31%
Early
Targeting
of
Minority
Students
75%
38%
URM
Student
Recruiters
71%
61%
Enrichment
Programs
66%
56%
Community
Based
Education
Programs
64%
39%
Alumni
Involvement
64%
33%
Application
Assistance
61%
37%
Partnerships:
Education
or
Labor
State
Departments,
Foundations
44%
36%
effective")
and
enrichment
programs
for
minority
stu-
dents
(56%
of
schools
rated
this
strategy
as
"very
effective").
However,
few
schools
(<15%)
rated
any
of
the
11
strategies
as
being
totally
ineffective.
Of
the
11
strategies,
the
only
one
positively
correlated
with
the
percentage
of
URM
students
was
having
summer
enrichment
programs.
Among
the
36
schools
that
reported
having
such
a
program,
the
mean
percentage
of
entering
URM
students
was
12.5%
±
6%
versus
7.0%
±
4.8%
(p<0.01)
at
the
20
schools
that
did
not
report
having
such
a
program.
Other
Underrepresented
Minorities
When
schools
were
asked
about
interest
in
recruit-
ing
other
groups,
86%
said
they
were
interested
in
recruiting
economically
disadvantaged
students,
58%
were
interested
in
the
recruiting
racial/ethnic
minori-
ties
not
currently
designated
as
URM,
57%
in
women
and
42%
in
students
with
disabilities.
Fewer
schools
were
interested
in
attracting
second-career
students
(36%)
or
gay
and
lesbian
students
(24%).
When
asked
in
an
open-ended
way
what
other
groups
the
schools
were
interested
in
targeting,
the
most
frequent
answer
was
in
recruiting
regional
ethnic
minorities.
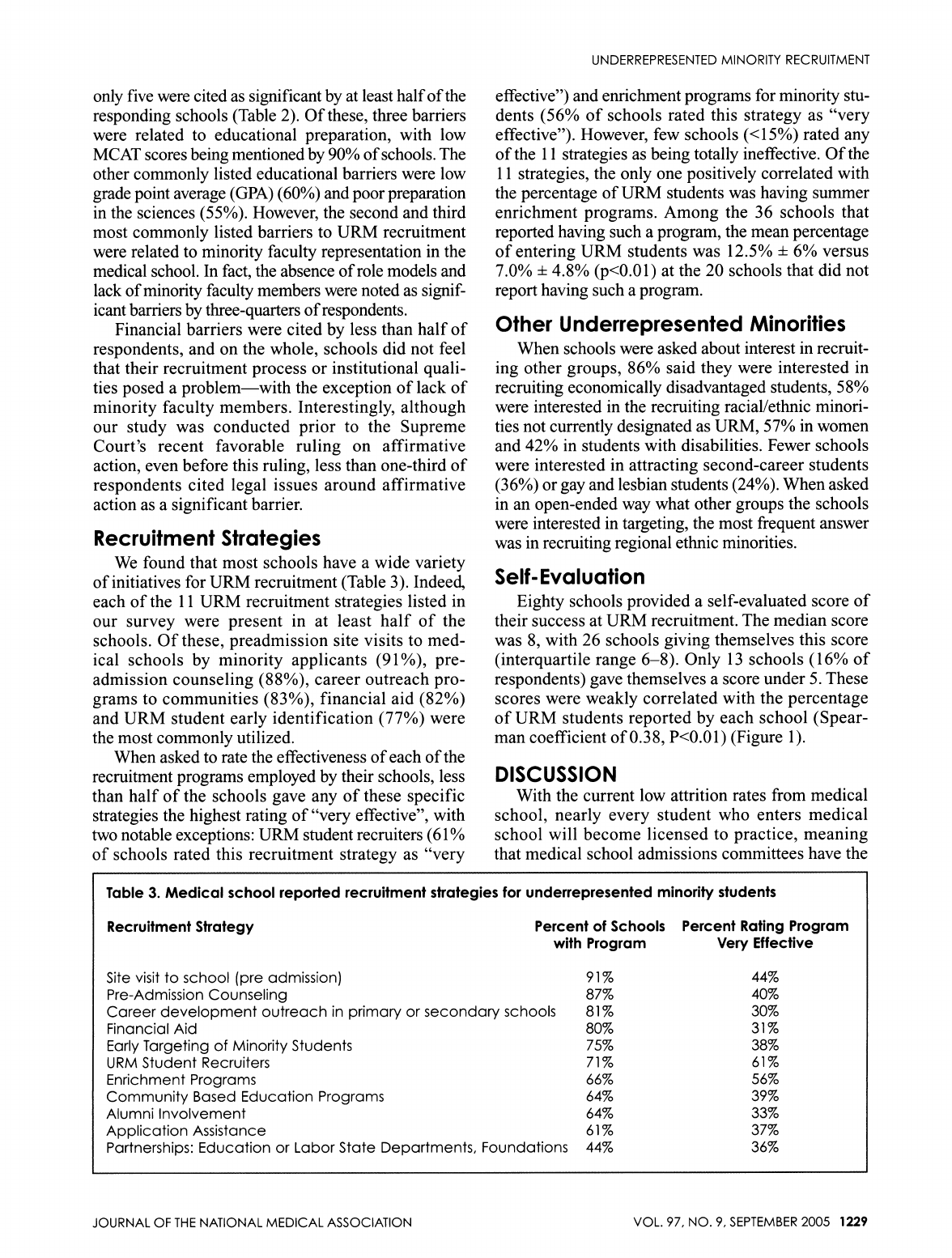
Self-
Evaluation
Eighty
schools
provided
a
self-evaluated
score
of
their
success
at
URM
recruitment.
The
median
score
was
8,
with
26
schools
giving
themselves
this
score
(interquartile
range
6-8).
Only
13
schools
(16%
of
respondents)
gave
themselves
a
score
under
5.
These
scores
were
weakly
correlated
with
the
percentage
of
URM
students
reported
by
each
school
(Spear-
man
coefficient
of
0.38,
P<0.01)
(Figure
1).
DISCUSSION
With
the
current
low
attrition
rates
from
medical
school,
nearly
every
student
who
enters
medical
school
will
become
licensed
to
practice,
meaning
that
medical
school
admissions
committees
have
the
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
97,
NO.
9,
SEPTEMBER
2005
1229

UNDERREPRESENTED
MINORITY
RECRUITMENT
sole
responsibility
of
choosing
the
nation's
future
physician
workforce.5
Our
study
examining
the
per-
ception
of
medical
schools
on
barriers
to
URM
recruitment
sheds
some
light
on
how
schools
make
admission
decisions
and
how
this
affects
diversity
in
the
classroom.
For
example,
low
GPA
and
MCAT
scores
among
URM
applicants
are
perceived
to
be
a
barrier
by
the
vast
majority
of
respondents,
suggest-
ing
that
schools
continue
to
place
significant
weight
on
these
admissions
criteria.
Concerns
regarding
overreliance
on
such
metrics
and
their
role
as
barriers
to
medical
school
diversity
have
existed
among
medical
educators
for
over
20
years.6
Yet
even
today,
expert
opinion
still
remains
divided
on
such
admissions
criteria,7-10
with
some
advocating
for
the
continued
role
of
the
MCAT
and
GPA
scores,
and
others
calling
for
the
abandonment
of
such
criteria
in
favor
of
"noncognitive
attributes"
(i.e.,
altruism,
maturity,
etc).
Most
recently,
the
Sul-
livan
Commission
on
Diversity
in
the
Health
Work-
force
recommended:
"medical
schools
should
reduce
their
dependence
upon
standardized
tests
in
the
admissions
process
...
and
the
MCAT
should
be
utilized
along
with
other
criteria
in
the
admissions
process
as
diagnostic
tools
to
identify
areas
where
qualified
health
professions
applicants
may
need
academic
enrichment
and
support."3
Our
study
also
underscores
the
importance
of
visi-
ble
URM
medical
school
faculty
and
students
in
the
building
of
a
diverse
physician
workforce
for
the
future.
Consistent
with
prior
reports,'
""2
a
large
propor-
tion
of
schools
noted
the
effectiveness
of
URM
stu-
dents
in
recruitment
and
the
absence
of
minority
facul-
ty
as
the
biggest
institutional
barrier
to
URM
recruitment.
However,
achieving
diversity
among
fac-
Figure
1.
Medical
school
self-evaluated
success
at
underrepresented
minority
student
recruitment
versus
the
percentage
of
entering
students
who
are
URM
30
l:
-
25-
a)*
2
20
-
15
-
z
0~~~~~~~~~~~~~
z-
*
102
S
)
*
2
a)
5-
*
t
a.
t,
t,
0
1
2
3
4
5
6
7
8
9
10
Spearman
coefficient
0.38,
P<0.01
Self-Rated
Success
ulty
at
medical
schools
has
proved
challenging,
with
URM
faculty
currently
representing
only
4.2%
of
med-
ical
school
faculty.4
Even
when
traditional
academic
productivity
metrics,
such
as
grants
and
publications,
are
adjusted
for,
studies
have
consistently
found
that
URM
faculty
are
less
likely
to
be
promoted.13'14
Further,
our
data
on
recruitment
programs
for
URM
students
suggests
that
most
medical
schools
employ
a
wide
variety
of
initiatives
to
encourage
applications
and
enrollment
by
URM
students.
However,
aside
from
summer
enrichment
programs
and
URM
student
recruiters,
schools
felt
that
most
other
programs
were
only
moderately
effective.
When
combined
with
the
data
on
barriers,
it
is
striking
that
recruitment
efforts
do
not
seem
to
directly
focus
on
the
barriers
identified
by
the
majority
of
schools:
faculty
diversity
and
the
strong
emphasis
that
schools
continue
to
place
on
MCAT
and
GPA
scores
as
admissions
criteria.
Lastly,
we
found
that
the
majority
of
medical
schools
tended
to
rate
themselves
highly
with
respect
to
their
performance
in
creating
a
diverse
student
body.
It
is
unclear
how
schools
evaluated
themselves,
as
we
found
only
weak
correlation
between
self-rated
success
scores
and
the
percentage
of
new
URM
stu-
dents.
As
most
schools
believe
they
are
doing
rather
well
at
URM
recruitment,
this
finding
suggests
that
many
schools,
on
their
own,
may
not
aggressively
pursue
the
additional
requisite
changes
needed
to
achieve
a
more
diverse
physician
workforce.
Limitations
to
our
study
include
the
low
response
rate
as
well
as
possible
discrepancies
between
the
med-
ical
schools'
views
on
URM
recruitment
and
those
of
other
groups,
such
as
students.
For
example,
while
stu-
dents
often
cite
lack
of
financial
resources
as
a
barrier
to
entering
and
succeeding
in
medical
school,'5"16
less
1230
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
97,
NO.
9,
SEPTEMBER
2005

UNDERREPRESENTED
MINORITY
RECRUITMENT
than
half
the
schools
in
this
study
felt
that
lack
of
finan-
cial
aid
or
parental
income
was
a
problem.
Our
nation
has
embarked
on
an
ambitious
agenda
of
eliminating
the
glaring
racial
and
ethnic
in-
equities
that
exist
in
our
healthcare
system.
Achiev-
ing
physician
workforce
diversity
will
be
an
impor-
tant
step
towards
achieving
this
goal,
and
our
study
shows
that
schools
are
investing
tremendous
efforts
into
minority
recruitment.
However,
our
study
also
suggests
that
current
initiatives
may
not
be
address-
ing
the
central
barriers
that
schools
themselves
iden-
tify-admissions
criteria
and
URM
presence
among
the
faculty.
Of
note,
these
are
institutional
barriers,
directly
amenable
to
intervention
by
the
schools
themselves.
Furthermore,
our
study
also
suggests
that
schools
may
have
difficulty
with
internal
evalu-
ation
of
their
recruitment
efforts,
perhaps
underscor-
ing
the
need
for
an
external
body
to
assist
with
the
development
of
diversity
goals
and
an
evaluation
of
their
performance.
Until
these
critical
issues
are
addressed,
we
fear
that
efforts
to
achieve
a
more
diverse
workforce
will
remain
at
an
impasse.
ACKNOWLEDGEMENTS
We
thank
Dr.
Nathan
Stinson
and
Jim
Simpson
of
the
OMH,
Mr.
Paul
Wright
of
AMSA,
Joan
Hedge-
cock
of
the
AMSA
Foundation,
Dr.
PJ
Maddox
and
Victoria
Doyon
of
George
Mason
University,
and
the
participants
on
the
AMSA
Diversity
Coalition
for
their
input
into
survey
development.
The
comments
in
this
manuscript
do
not
neces-
sarily
reflect
the
views
of
AMSA,
OMH,
NCMHD
nor
the
universities
or
hospitals
with
which
the
authors
are
affiliated.
REFERENCES
1.
Minority
students
in
medical
education:
facts
and
figures.
Washington,
DC:
Association
of
American
Medical
Colleges,
2002.
www.aamc.org/
publications/medicalschoolmatriculants.pdf.
2.
Overview
of
race
and
Hispanic
origin,
census
2000
brief.
Washington,
DC:
U.S.
Census
Bureau
Publication
#C2KBR/01-1;
2001.
Available
at
www.census.gov/prod/2001
pubs/c2kbrOl-1
.pdf.
3.
Missing
persons:
Minorities
in
the
Health
Professions.
Durham,
NC:
The
Sul-
livan
Commission
of
Diversity
in
the
Health
Workforce,
2004.
http://admis-
sions.duhs.duke.edu/sullivancommission/documents/Sullivan
Final-Report
_000.pdf.
4.
In
the
nation's
compelling
interest.
Ensuring
diversity
in
the
health
profes-
sions.
Washington,
DC:
National
Academy
of
Sciences
Press,
2004.
www.nap.edu/books/0309091
25X/html.
5.
McGaghie
W.
Perspective
on
medical
school
admission.
Acad
Med.
1990;65:136-139.
6.
Shea
S,
Fullilove
MT.
Entry
of
black
and
other
minority
students
into
U.S.
medical
schools.
Historical
perspective
and
recent
trends.
N
Engl
J
Med.
1985;313:932-940.
7.
Edwards
JC,
Elam
CL,
Wagoner
NE.
An
admission
model
for
medical
schools.
Acad
Med.
2001;76:1207-1212.
8.
Jones
BJ,
Borges
NJ.
The
contribution
of
noncognitive
characteristics
in
predicting
MCAT
scores.
Acad
Med.
2001;76:S52-S54.
9.
Albanese
MA,
Snow
MH,
Skochelak
SE,
et
al.
Assessing
personal
qualities
in
medical
school
admissions.
Acad
Med.
2003;78:313-321.
10.
Miller
HC.
Affirmative
Action
in
Medical
School
Admissions.
JAMA.
2003;289:3085-3086.
1
1.
Cregler
LL.
A
second
minority
mentorship
program.
Acad
Med.
1993;
68:148.
12.
Shields
PA.
A
survey
and
analysis
of
student
academic
support
pro-
grams
in
medical
schools,
focus:
underrepresented
minority
students.
J
NatI
Med
Assoc.
1994;86:373-377.
13.
Fang
D,
Moy
E,
Colburn
L,
et
al.
Racial
and
ethnic
disparities
in
faculty
promotion
in
academic
medicine.
JAMA.
2000;284:1085-1092.
14.
Palepu
A,
Carr
PL,
Friedman
RH,
et
al.
Minority
faculty
and
academic
rank
in
medicine.
JAMA.
1998;280:767-771.
15.
The
color
of
medicine:
strategies
for
increasing
diversity
in
the
U.S.
physi-
cian
workforce.
Boston:
Community
Catalyst,
2002.
www.community
cat.org/acrobat/The-Color_of_Medicine.pdf.
16.
Study
group
on
minority
medical
education.
Reston,
VA:
The
American
Medical
Student
Association,
1996.
www.amsa.org/pdf/study_meded.PDF.
A
We
Welcome
Your
Comments
The
Journal
of
the
National
Medical
Association
welcomes
your
Letters
to
the
Editor
about
articles
that
appear
in
the
JNMA
or
issues
relevant
to
minority
healthcare.
Address
correspondence
to
C
A
f
The
University
of
California,
Davis
School
of
Medicine
is
recruiting
for
faculty
members
at
the
Assistant/Associ-
ate/full
Professor
level
in
several
of
its
clinical
and
basic
science
departments.
These
include
positions
with
research,
teaching,
and/or
clinical
responsibilities
in
any
of
our
five
academic
series.
Specific
details
on
positions
including
required
educational
degrees,
experience,
and
responsibilities,
and
the
individual
to
contact
for
sub-
mission
of
an
application
can
be
found
at
the
following
website:
http://provost.ucdavis.edu/cfusion/emppost/
search.cfm
The
University
of
California,
Davis
is
an
affirmative
action/
equal
opportunity
employer
with
a
strong
commitment
to
achieving
diversity
in
its
faculty
and
staff.
OB/Gyn
Needed
in
San
Francisco
Bay
Area
O.AKCARE
A
BC/BE
OB/Gyn
is
needed
for
an
IMEDICAL
exciting
position
in
a
growing
GROUP
Maternal
Child
Health
department
at
a
County
Medical
Center
serv-
ing
diverse
populations.
The
OB/Gyn
will
be
required
to
perform
varied
services
in
Labor
&
Deliv-
ery,
Urgent
Care
and
clinics.
There
are
approxi-
mately
12
OB/Gyn
FTEs
serving
this
population.
We
offer
competitive
salaries
with
good
benefits.
Please
send
CV
to
Vishu
Lalchandani,
CAO,
Oak-
Care
Medical
Group,
Fax
(510)
437-9651
or
phone
(510)
437-4293
for
more
information.
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
97,
NO.
9,
SEPTEMBER
2005
1231
